Abstract
Background:
The Coronavirus-19 is an ongoing global pandemic that to date, has resulted in over 5 million deaths with more than 240 million cases worldwide. COVID-19 has caused a major burden on public health; however, it simultaneously shed the light on pre-existing gaps within current health care systems worldwide. Health care systems were burdened through both inpatient as well as outpatient settings, with a notable decline in outpatient clinic follow ups. Fortunately, many innovated solutions were being created to tackle the may barriers, one being telehealth. Telemedicine is the provision of medical information exchanged via electronic communication. This is done through a growing variety of services, such as audio or video calls, emails, and other forms of telecommunication. It is a promising means that can provide care to a selected group of patients, particularly cancer patients who are at a higher risk in comparison to the general population. It provides a safe and alternative route to combat patient care while minimizing their risk of exposure. In this study we provide insight to patients experience with telemedicine through this pandemic.
Methods:
We conducted a cross-sectional study on 279 (RR:85%) patients in tertiary cancer care center National Center for Cancer Care and Research (NCCCR) in Qatar. Our inclusion criteria included patients following regularly by telemedicine in outpatient clinics during COVID 19, patients aged 18 years and above, ability to complete the questionnaire over the phone and with no language barriers. We excluded patients who did not respond to the phone call after 5 attempts (at different times on different days), patients who were abroad, patients who did not consent to answer the questionnaire and patients who had expired. Data was collected through phone calls whereby a standard introductory script followed by a survey questionnaire was read by the physician to patients. We focused on patients' experience with telemedicine services amid the pandemic. This was done by using 7 questions that were scaled from 1 through 6, using a six-point Likert scoring system. It was divided into two main categories; category 1 comprised of patients' demographics and category 2 comprised of 7 questions on their feedback and satisfaction scale.
Results:
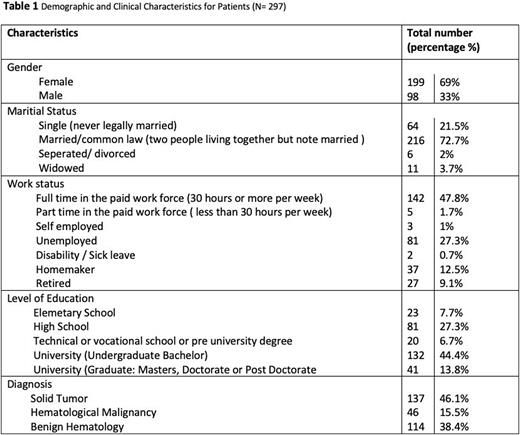
Over a period of 6 weeks, 297 patients were contacted over the phone to answer the survey questionnaire (Table 1). The cohort of patients included 46.1% with solid tumor malignancy, 38.4% with benign hematological conditions and 15.5% with hematological malignancies. More than 80% of patients somewhat to strongly agreed that telemedicine met their care needs, improved their confidence in their health care system, and were generally satisfied with the quality of care provided. It was evident that the level of communication through telemedicine was not compromised over the phone as 89% of patients somewhat to strongly agreed they could freely talk; 90% understood their physicians' recommendations and more than half of the patients (89%) felt they could freely communicate their concerns. Although 88% of participants were somewhat to strongly satisfied with their telemedicine experience; if given the choice most would prefer in person consultations over teleconsultations (68% vs. 32%, respectively). Having said that, 90% would still be willing to take part in future teleconsultations.
Conclusions:
Telemedicine is a revolutionary system that has pioneered a new era for delivering patient care. Integration of telemedicine-based care into our standard practices in the future, could potentially provide a safe health care system in addition to being time and cost-effective for health sectors and patients alike. Our study indicates an overall positive experience among patients towards the use of telemedicine. Although our data did show that patients preferred in-person visitations majority were not opposed to future teleconsultations. Cancer care providers may explore the reasoning as well as solutions for this with future studies. We as health care professionals should look to implementing patient as well as physician education so that we may expand the telehealth approach in the future.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal